CME CASE 1
40 YEAR OLD FEMALE WITH PERIORBITAL PUFFINESS
** This is an ongoing case. I am in the process of updating and editing this ELOG as and when required.
Note: This is an online E Log book recorded to discuss and comprehend our patient's de-identified health data shared, AFTER taking his/her/guardian's signed informed consent.
Here, in this series of blogs, we discuss our various patients' problems through series of inputs from available global online community of experts with an aim to solve those patients' clinical problems, with collective current best evidence based inputs.
This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end.
I have been given the following case to solve, in an attempt to understand the concept of "Patient clinical analysis data" to develop my own competence in reading and comprehending clinical data, including Clinical history, Clinical findings, Investigations and come up with the most compatible diagnosis and treatment plan tailored exclusively for the patient in question.
CASE :
Chief complaint:
-Puffiness around eyes since 2months
-Tingling all over the head since 2 months
- shortness of breath since 2 months
-joint pains since 2 months
History of present illness:
- Patient was apparently symptomatic 2 months ago then she developed puffiness of eyes aggravating with work and cold temperature , revealing on taking rest.
- Not progressing, no diurnal variations.
- Patient chief complaint of tingling all over the head since 2 months aggravating with sleep. No relieving factors.
- Patient had neck pain since 2 months and restriction of movement
- Patient complaints of difficulty breathing. Aggravating with mild daily routine activities , No seasonal variation, no allergies
- Patient complaint of Body pains Over the large joints Since two months, no history of abdominal pains burning micturItion deviation of mouth, squint , dysphagia
- Patient wakes up at 5:00 am
- She makes tea for herself and her son and have at 6:00 am
- She will do all household work works and prepare lunch till 9 am
- At 9 am she will have rice and some curry as breakfast
- she will go to work i.e plucking cotton (harvesting) after having breakfast
- At 2pm she will have her lunch rice and curry
- She will have dinner at 8:00 pm with rice, curry and curd
- She will go to sleep by 9:00 pm
Past history:-
Not a known case of DM,HTN,EPILEPSY, CVD,CAD
past history of trauma to left temporal side of head
Personal history:
Married, daily wage worker
Normal appetite , regular bowel and bladder movements
No allergies
no addictions
Family history: Not Significant
Menstrual history:
Age of menarche: 13 yrs
LMP : 1/12/23
OBSTETRIC HISTORY:
Age at marriage:7 yrs
age at 1st child birth:19yrs
G2P2
General examination:
Patient is conscious coherent cooperative
Pallor present
No icterus, cyanosis, clubbing, lymphadenopathy, malnutrition, dehydration
Vitals:
Temperature 98°F
Pulse rate: 84 bpm
Respiratory rate: 22cpm
Blood pressure: 100/60mmHg
SpO2 98%
Systemic examination :
CVS:
S1 , S2
no murmurs
no thrills
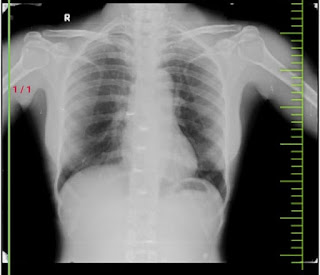
Respiratory system:
trachea central
bilateral air entry present
normal vesicular breath sounds heard
Abdomen examination:
scaphoid shape
no tenderness, no palpable mass
liver and spleen not palpable
no bowel sounds heard
no bruits heard
Central nervous system:
patient is conscious
speech- normal
no focal neurological deficiet
higher mental functions are intact
Reflexes:
RIGHT LEFT
Biceps - ++ ++
Triceps- ++ ++
supinator- + +
knee - ++ ++
ankle- + +
Differential diagnosis:
• Nephrotic syndrome
• Beri beri
• Anemia induced high output cardiac failure
Investigation:
Blood grouping
Random blood glucose
Fasting blood glucose
Post prandial blood glucose